Mpox Update
Initial Outbreak
In July of 2022, the World Health Organization (WHO) declared an outbreak of mpox, at the time referred to as “monkeypox”, a Public Health Emergency of International Concern. Mpox is endemic to some African countries and can spread from animals (natural hosts include African rodents such as squirrels and rats) to humans. The disease is spread to other regions by human travelers.
Disease Spread, Incubation Period, and Symptoms
Mpox usually spreads through skin-to-skin and sexual contact. Although less common, mpox can spread by touching objects, fabrics, and surfaces that have been used by someone with mpox. People with mpox often get a rash that may be located on hands, feet, chest, face, or mouth or near the genitals, including penis, testicles, labia, and vagina, and anus. It can take 3–17 days for symptoms to show after becoming infected (the incubation period). The full list of possible mpox symptoms include:
- Rash
- Fever
- Chills
- Swollen lymph nodes
- Exhaustion
- Muscle aches and backache
- Headache
- Respiratory symptoms (e.g., sore throat, nasal congestion, or cough)
To learn more about the signs and symptoms of mpox visit: Signs and Symptoms of Mpox | Mpox | CDC
To see photos of what mpox rashes can look like, visit: Photos of mpox rashes
Clades I and II
There are two know subtypes of mpox: Clade I, which is endemic to Central Africa, and Clade II, which is endemic to West Africa and continues to spread at low levels in many countries throughout the world, including the United States. While you can’t tell which kind of mpox someone has by looking at them, Clade I is more severe than Clade II and can cause higher mortality rates, especially in people who are immunocompromised. To better understand the differences between Clades I and II, view the following infographic from the Johns Hopkins Bloomberg School of Public Health: Mpox Outbreak Clade I vs. Clade 2.
What Is New: Clade I Identified in a Traveller in the United States
The California Department of Public Health confirmed, through laboratory testing, the first known case of clade I mpox in the United States in a person who had recently traveled from Eastern Africa. The patient has since been treated and their symptoms are improving. While the risk of clade I mpox to the public remains low, and there continue to be sporadic clade II mpox cases in the United States.
Mpox Guidance from the Centers for Disease Control and Prevention (CDC)
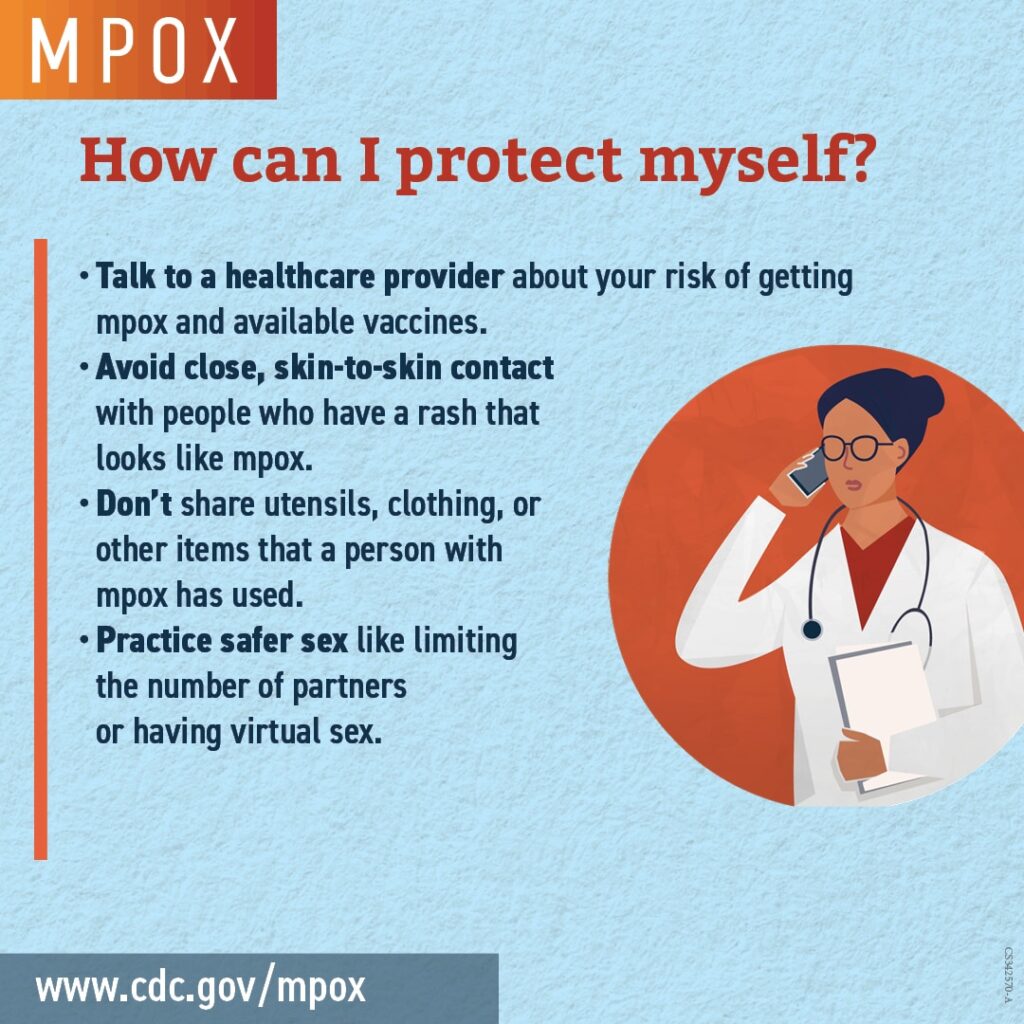
Guidance from CDC has not changed since the appearance of clade I mpox in the United States. Mpox infection can be prevented by:
- Vaccination–recommendations below
- Avoiding direct or skin-to-skin contact with people who have a rash that looks like mpox.
- Avoiding objects or materials a person with mpox has used.
- Avoiding wild animals in areas where mpox occurs regularly.
- Washing hands often and learning steps to lower your risk of mpox during sex or at social gatherings.
For further information on preventing mpox, visit: Preventing Mpox | Mpox | CDC
Mpox Vaccination

Vaccination is an important tool in stopping the spread of mpox!
The virus that causes mpox is related to the virus that causes smallpox. JYNNEOS is a 2-dose vaccine developed to protect against mpox and smallpox. People should get two doses of the vaccine for the best protection against mpox. The second dose should be given 4 weeks after the first dose. However, it is never too late to get your second dose. If it has been longer than 4 weeks since you got the first dose, get the 2nd dose as soon as possible.
CDC recommends vaccination for:
After a known exposure, also referred to as post-exposure prophylaxis (PEP) vaccination:
- You had known or suspected exposure to someone with mpox.
- You had a sex partner in the past 2 weeks who was diagnosed with mpox.
Before an exposure or pre-exposure vaccination (PrEP) in persons at risk for mpox:
- You are a gay, bisexual, or other man who has sex with men or a transgender, nonbinary, or gender-diverse person who in the past 6 months has had any of the following:
- A new diagnosis of one or more sexually transmitted diseases (e.g., chlamydia, gonorrhea, or syphilis)
- More than one sex partner
- You have had any of the following in the past 6 months:
- Sex at a commercial sex venue (like a sex club or bathhouse)
- Sex related to a large commercial event or in a geographic area (city or county for example) where mpox virus transmission is occurring
- You have a sex partner with any of the above risks
- You anticipate experiencing any of the above scenarios
- If you are traveling to a country with a clade I mpox outbreak and anticipate any of the following activities during travel, regardless of gender identity or sexual orientation:
- Sex with a new partner
- Sex at a commercial sex venue (e.g., a sex club or bathhouse)
- Sex in exchange for money, goods, drugs, or other trade
- Sex in association with a large public event (e.g., a rave, party, or festival)
- You are at risk for occupational exposure to orthopoxviruses (e.g., certain people who work in a laboratory or a healthcare facility).
When an individual at risk requests vaccine, they will not be asked which of these criteria applies. It is sufficient to say that they consider themselves to be at risk for mpox.
You should NOT get the mpox vaccine if:
You had a severe allergic reaction (such as anaphylaxis) after getting a previous dose of the JYNNEOS vaccine or to a vaccine component.
Talk to your healthcare provider if you had an allergic reaction to the antibiotics gentamicin or ciprofloxacin, or chicken or egg protein.
For more information about getting vaccinated for mpox, visit: Mpox Vaccination | Mpox | CDC.
Where to get an Mpox Vaccine on Cape Cod:
Mpox (Monkeypox) Resource Information – Outer Cape Health Services
AIDS Support Group of Cape Cod
Comprehensive List of Mpox Vaccine Locations in MA
Additional Resources: MPOX Information | Town of Provincetown, MA – Official Website
Source: CDC