Pertussis (Whooping Cough) on the Cape & Islands
Pertussis, also called “whooping cough”, is a common and highly contagious bacterial respiratory infection that can be dangerous, especially to young infants. In older children, teens, and adults, the symptoms of pertussis are often mild, but can last for weeks or months.
Pertussis lives in the nose, mouth, and throat of an infected person and is spread through the air by sneezing, coughing, or talking. Pertussis can also live on surfaces, so touching a tissue or sharing a cup used by someone with pertussis can effectively spread the disease. Pertussis can exacerbate the symptoms of people with pre-existing moderate-to-severe asthma, immunocompromising conditions, and possibly other conditions.
During the COVID-19 pandemic, respiratory protections like masking and remote work/learning led to decreases in transmission of pertussis. Post-pandemic, pertussis is back on the rise in Barnstable County, Massachusetts, and nationally. To-date, there have been no cases in Dukes or Nantucket counties.
Read the MA DPH Clinical Advisory regarding pertussis in Massachusetts >>>
This page includes information about:
- Symptoms of pertussis
- Pertussis prevention (vaccine)
- Pertussis epidemiology specific to the Cape & Islands
- Trends by age
- Trends by year and county
- Information for Healthcare Providers
- Optimal timing for pertussis diagnostic testing
- Requested actions
- Help stop the spread
Symptoms, Diagnosis, and Treatment of Pertussis
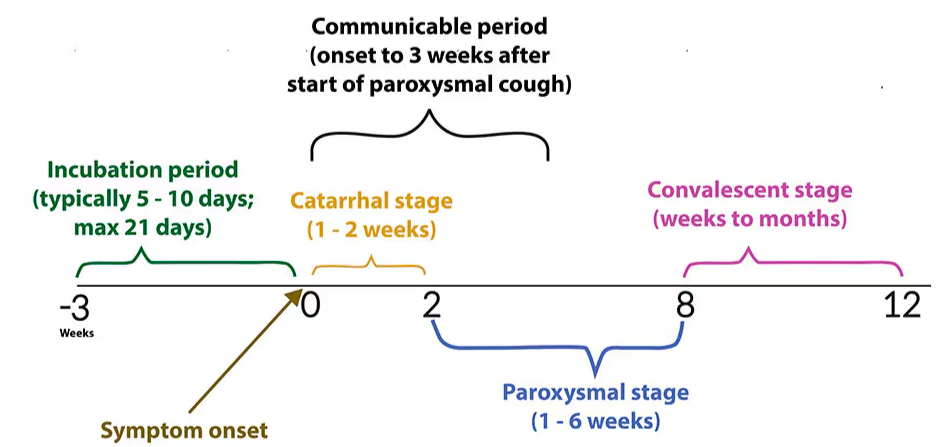
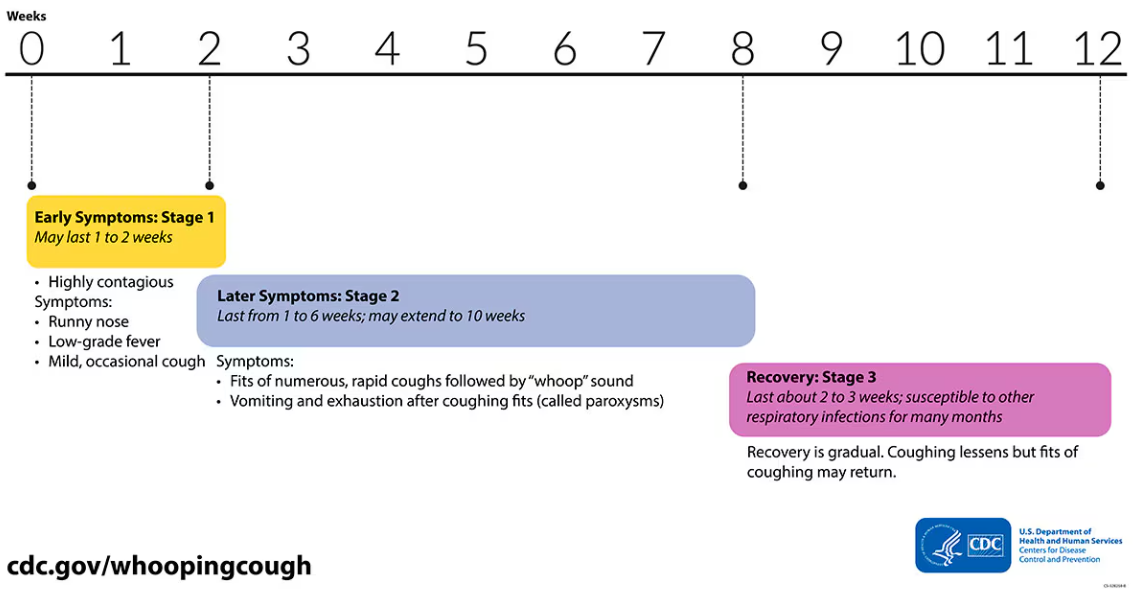
Pertussis has three stages, resulting in a progression of symptoms that can last weeks to months if left untreated:
- Week 1-2 (Catarrhal stage): Symptoms mimic the common cold including runny nose, sneezing, and mild cough.
- Weeks 2-8 (Paroxysmal stage): Symptoms progress to a worsening, miserable cough that can cause such severe coughing fits that people may become blue in the face or make a “whoop” sound as they try to catch their breath. Patients can become exhausted or begin vomiting from such severe coughing. Coughing attacks occur frequently at night.
- Weeks 8-12 (Convalescent stage): Symptoms gradually improve with less persistent coughing fits that disappear in 2 to 3 weeks.
Early Diagnosis and Treatment are Essential
Without antibiotic treatment, people who are sick with pertussis are most infectious to others in the first 3 weeks of symptoms. So early diagnosis and treatment are essential. After 5 days of antibiotic treatment, the sick person is no longer contagious to anyone else. Early administration of antibiotics can also reduce the length and severity of symptoms.
If You Have Been Exposed to Pertussis, Talk to Your Doctor about Treatment Before Symptoms Start
If someone has close contact with someone with pertussis and they get infected, symptoms usually start showing up 5 to 10 days later but could take as long as 21 days. In that window, there is the option to take 5 days of antibiotics to altogether prevent getting pertussis at all. This is recommended for household contacts who are highly likely to get pertussis from their family member. This can also be very important if you are high risk for severe illness or could have contact with high risk individuals (see below about infants and pregnant women). If you have been exposed to pertussis, call your doctor and ask about “prophylaxis“.
Pertussis is Especially Concerning for Infants
In babies, pertussis can cause breathing problems, pneumonia, and swelling of the brain (encephalitis), which can lead to seizures and brain damage. In rare cases pertussis can even be fatal, especially in very young infants.
The following video from the Mayo Clinic, while difficult to watch, shows the effects of pertussis in a young infant: Infant girl with whooping cough (youtube.com)
Pregnant Women in their Third Trimester
It is important to protect and/or treat pregnant women so that they do not inadvertently infect their infants post-birth.
If you think you or a loved one has pertussis, or has been exposed to pertussis, talk to a doctor as soon as possible!
Pertussis can be PREVENTED!
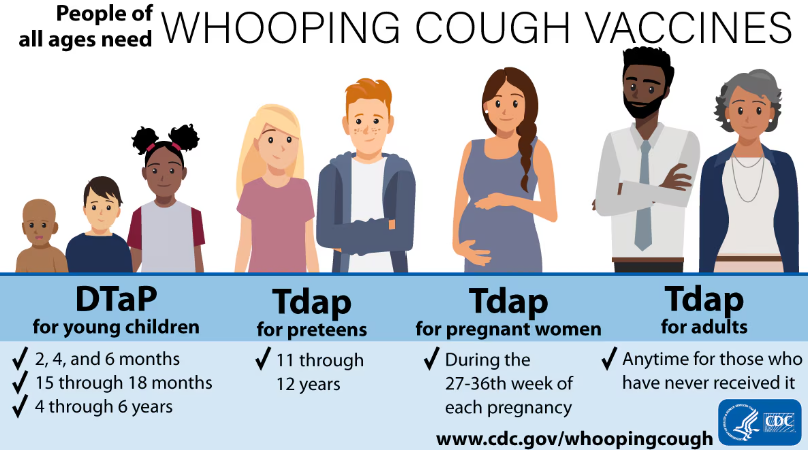
Pertussis vaccines are the best way to protect against whooping cough! The Centers for Disease Control and Prevention recommends pertussis (whooping cough) vaccination for everyone.
Talk to a vaccine provider if you have questions about pertussis vaccine. Many pediatricians, doctor’s offices, and pharmacies offer pertussis vaccines. Barnstable County Public Health Nurses also offer the vaccine. Appointments are available on Tuesdays and Thursdays 8:30am to 4:00pm. To schedule an appointment, call (508) 375-6617.
In the following video, Michael Forbes, MD, an intensivist in the pediatric intensive care unit at Akron Children’s Hospital, discusses the symptoms of this disease, as well as its treatment and prevention.
Pertussis (whooping cough) - Akron Children's Hospital video
Pertussis Epidemiology on the Cape & Islands
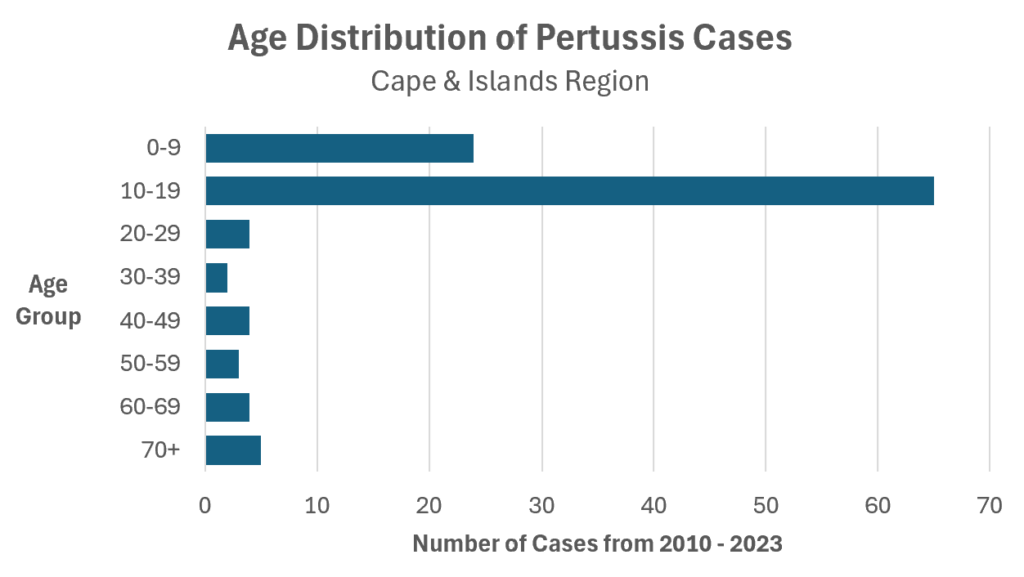
Pertussis Trends By Age
Since 2010, approximately 80% of diagnosed and reported pertussis cases on the Cape & Islands have been in kids and teenagers.
Pertussis Trends by Year and County
YTD = Year-to-Date. Last updated October 14, 2024
Includes confirmed and probable cases. Date assigned is based on the date symptoms started. If a patient is unable to be interviewed to determine symptom onset date, the date the individual first tested positive is used. Learn more about how public health officials classify cases here: Pertussis National Case Classification.
Because Dukes County and Nantucket County have smaller year-round populations (<25,000 people), years with fewer than 5 cases are reported as “<5” to preserve patient confidentiality.
| Year | Barnstable County (Cape Cod) | Dukes County (Martha's Vineyard & Elizabeth Islands) | Nantucket County (Nantucket, Tuckernuck) |
|---|---|---|---|
| 2024 (YTD*) | 10 | 0 | 0 |
| 2023 | 0 | 0 | 0 |
| 2022 | 0 | 0 | 0 |
| 2021 | 0 | 0 | 0 |
| 2020 | 0 | 0 | 0 |
| 2019 | 7 | 0 | 0 |
| 2018 | 3 | <5 | <5 |
| 2017 | 6 | 0 | 0 |
| 2016 | 0 | 0 | 0 |
| 2015 | 10 | <5 | 0 |
| 2014 | 42 | 0 | 0 |
| 2013 | 1 | <5 | 0 |
| 2012 | 23 | <5 | <5 |
| 2011 | 3 | 0 | 0 |
| 2010 | 5 | 0 | 0 |
Information for Health Care Providers
Optimal Timing for Pertussis Diagnostic Testing

Actions Requested of Healthcare Providers:
- Maintain a high index of suspicion for pertussis to identify those infected. It is recommended that providers consider pertussis in any patient of any age with prolonged cough, regardless of vaccination status.
- Test patients who have symptoms of pertussis (see Clinical Timing graphic for testing recommendations). PCR may be the more clinically useful option in early illness as it is readily available from hospital and commercial labs and results are available quickly. Still, CDC and MDPH recommend the use of PCR together with culture for the diagnosis of pertussis. Note that culture testing requires special ordering from the State Public Health Lab (use the Specimen Submission Form). Serology should be considered when appropriate.
- Initiate treatment promptly. The earlier antibiotics are started, the more effective they are at preventing transmission and possibly modifying illness. Consider treating prior to test results if clinical history strongly suggests pertussis, person is at high risk for severe or complicated disease, or person has or will have contact with someone at high risk for severe disease (see CDC Clinical Treatment recommendations).
- Inform patients with pertussis that they need to isolate and NOT participate in public activities (including work/school/camp) until they have completed 5 days of appropriate antibiotic treatment.
- Ask about close contacts.
- Close contacts with symptoms should also be treated as soon as possible and excluded from public activities until they have completed 5 days of antibiotic treatment.
- Close contacts without symptoms should receive prophylactic antibiotics to prevent infection with pertussis. Close contacts without symptoms do not need to be excluded from activities. If close contacts refused antibiotic prophylaxis, they should be educated on seeking care immediately should early pertussis symptoms develop (runny nose, sneezing, cough).
- Inform the Infection Control staff in your clinic of your patient with suspect pertussis.
- Report cases and provide information to public health authorities as soon as possible especially if the patient is in congregate settings like schools, camps, daycares, long-term care, jails, or indoor workspaces where public health investigation and intervention can prevent the spread of disease. Cough onset date, symptoms, and vaccination history help us determine whether formal public health control recommendations should be made.
- If you identify a case of pertussis, please report the individuals name, contact information, cough onset date, symptoms, testing performed, and vaccination history to your local board of health or the Massachusetts Department of Public Health at (617) 983-6800.