Do You Need a Measles Vaccine?
The best protection against measles is knowing IF you were vaccinated, WHEN you were vaccinated, and whether you should get a Measles, Mumps, & Rubella (MMR) vaccine. Most people who […]
Read MoreNOTICE: Temporary Office Closure for Cape Cod Cooperative Extension March 3rd – March 28th due to road construction.

Although measles was declared eliminated in the United States in 2000, cases have resurged in recent years due to declining vaccination rates. Recent outbreaks have been linked to travel-related cases that reached at-risk populations (populations with unvaccinated or under-vaccinated individuals).
Measles is EXTREMELY Contagious and Sometimes Dangerous
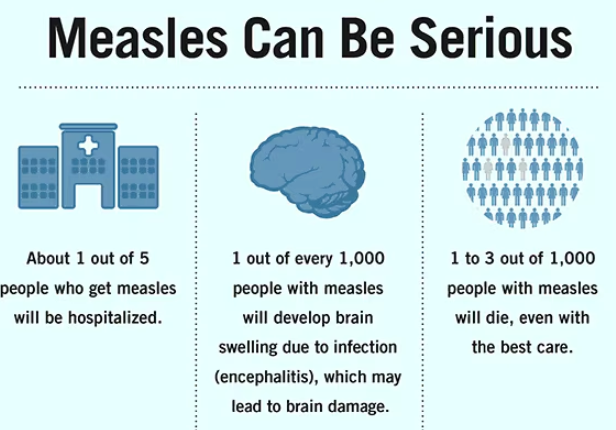
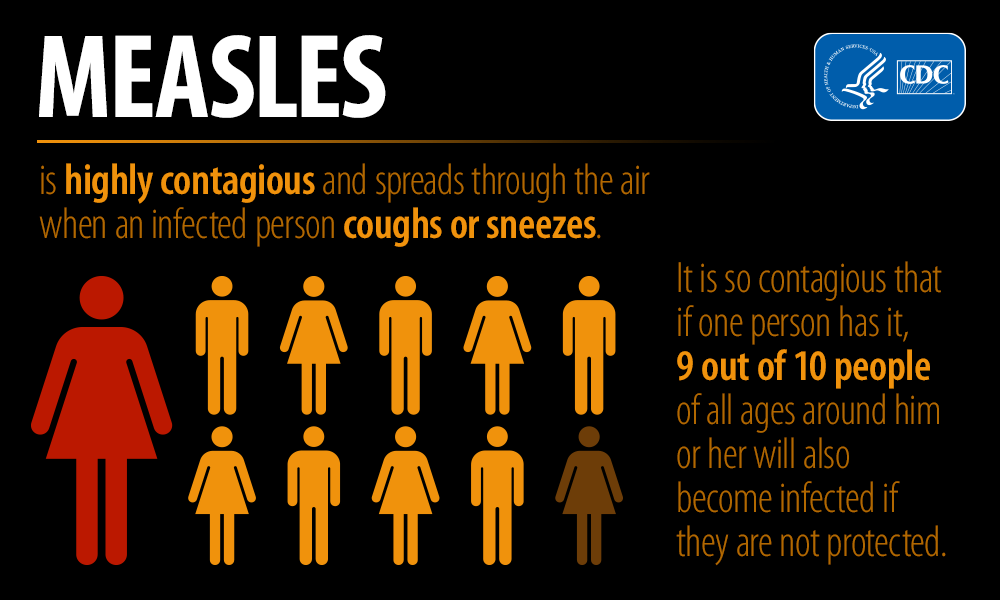
Measles is more easily spread than almost any other disease. The virus that causes measles lives in the nose and throat and is sprayed into the air when an infected person sneezes, coughs or talks. It can stay in the air for up to 2 hours. Other people nearby can then inhale the virus. Measles can have dangerous health complications for at risk groups, especially children under 5 years old.
In 2024: The U.S. reported 285 confirmed cases across 33 jurisdictions. Massachusetts had a single case in an adult with unknown vaccination history who had known close contact to a confirmed measles case during international travel. There have been no cases on Cape Cod and the Islands.
In 2025: As of March 13, 2025, a total of 301 measles cases were reported by 15 jurisdictions: Alaska, California, Florida, Georgia, Kentucky, Maryland, New Jersey, New Mexico, New York City, New York State, Pennsylvania, Rhode Island, Texas, Vermont, and Washington. There have been two deaths (one confirmed to be a result of measles and one death under investigation); 17% of cases have been hospitalized. There have been no cases to-date in Massachusetts.
It critically important for you to call your doctor’s office or hospital before going into the building. They will give you instructions on how you will enter the building so you can be evaluated safely. This is extremely important to prevent infecting other people while you seek care.

On March 11, 2025, Massachusetts Department of Public Health put out a clinical advisory and update regarding the spread of measles in the United States.


Measles is a virus that infects the lungs and breathing passages like the nose, mouth, and throat, and spreads throughout the body.
Anyone who is not already immune can contract measles, but it most commonly affects children. Certain groups are most at risk for serious measles complications, including:
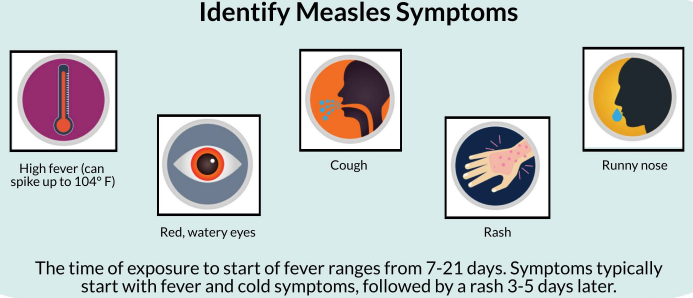
Measles symptoms can include:
For pictures of measles rash or Koplik spots, visit: Photos of Measles.
Measles is highly contagious. An infected individual can spread the disease to others before noticing any symptoms, especially in the four days before and after a rash develops. Measles virus is exhaled by the infected person and can remain suspended in the air for 2 hours, even after the infected person leaves the room.
Data show that unvaccinated people have a 90% likelihood of contracting measles if exposed. Unvaccinated children who have not previously been infected are more likely to get infected.
There is no treatment for measles, but you can take actions to feel better and prevent complications. If you or your child has measles or believe you have been exposed, isolate yourself away from others and call a healthcare provider immediately. Hydration, rest, avoiding harsh light, and taking a fever reducer or pain reliever can also help relieve symptoms.
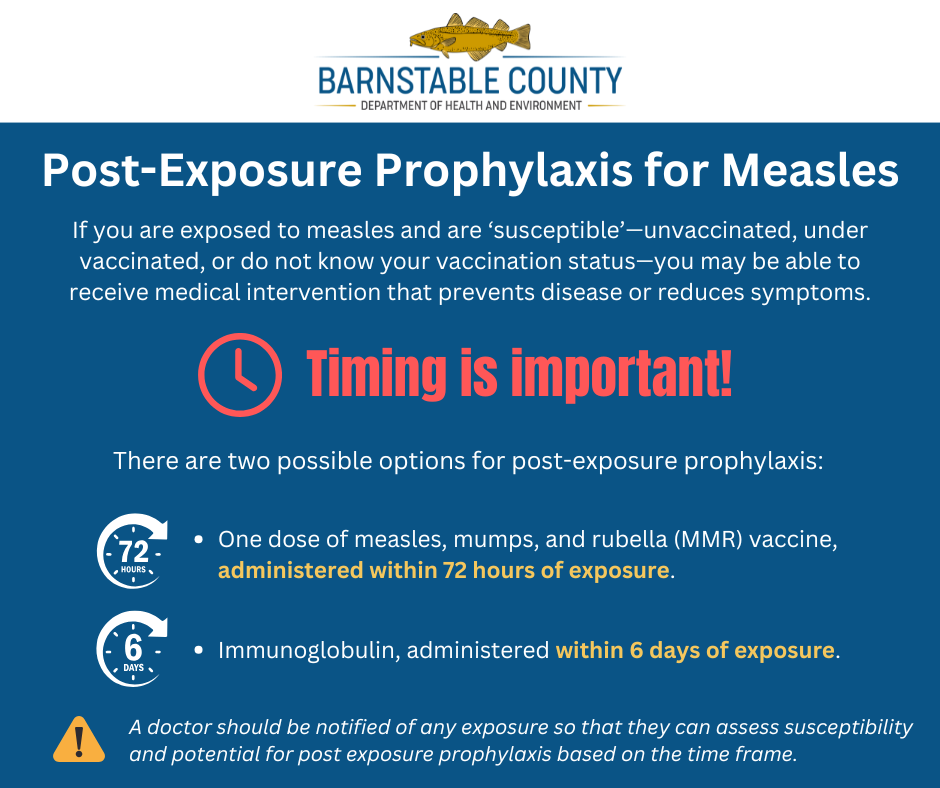
Exposed individuals can prevent measles if action is taken quickly post exposure. Those who do not have evidence of immunity and have had a known exposure to measles should call their doctor immediately. They may give you post-exposure prophylaxis (medical treatment that prevents or reduces severity of disease).
There are two possible options for post-exposure prophylaxis (remember, timing is important):
A doctor should be notified of any exposure so that they can assess susceptibility and potential for post exposure prophylaxis based on the time frame.
After an exposure, it can take anywhere from 7 to 21 days for the symptoms of measles to appear. Most commonly, symptoms appear 10 to 14 days after exposure. The first symptom is usually fever. The measles rash typically begins 2 to 4 days after the fever begins.
If you are susceptible—unvaccinated or under vaccinated for measles AND have travelled internationally or to places in the United States with known outbreaks—monitor your health for 21 days after returning home. It is 90% likely that a susceptible person will get measles after being exposed.
If you develop signs or symptoms of measles, call your doctor immediately and inform them that you were in a location where measles was transmitting. Your doctor will provide instructions on how to come into the clinic or hospital to be evaluated safely without exposing other people.
Information regarding known outbreaks:
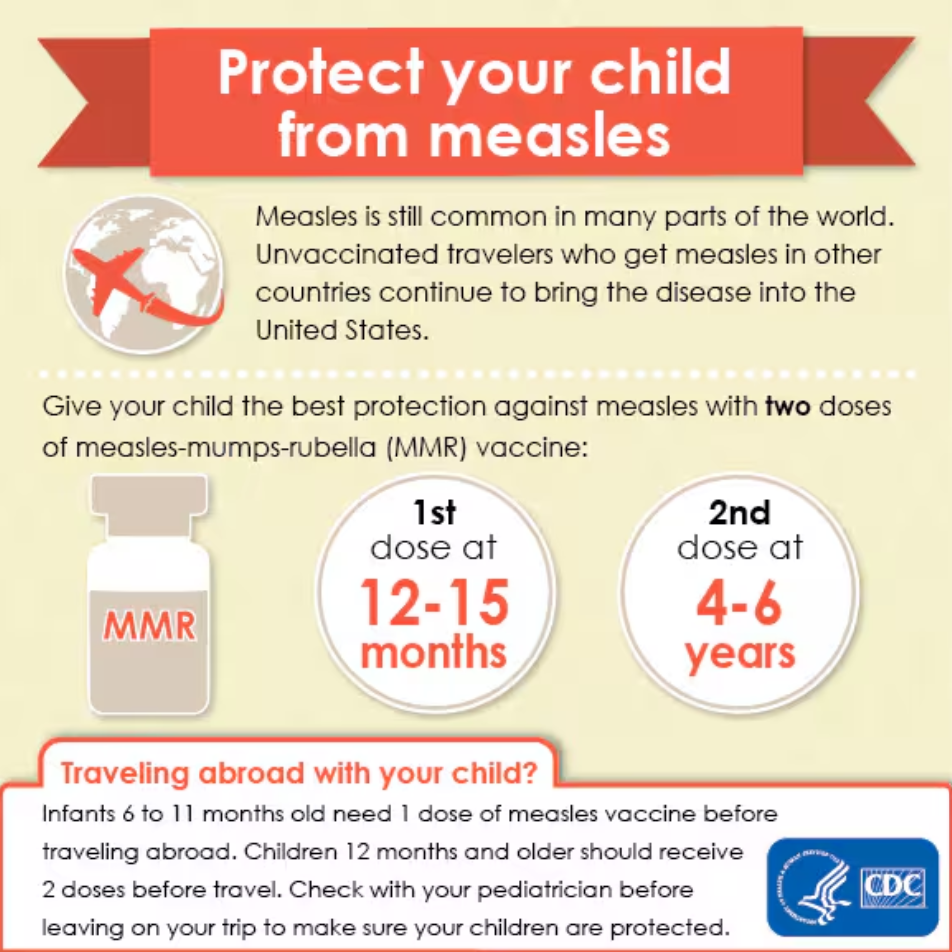
Vaccination is the most effective way to avoid contracting measles. CDC data show the measles-mumps-rubella (MMR) vaccine is highly effective and safe. Individuals with a history of prior infection or vaccination who have received the full two-dose series of MMR vaccines are 97% protected and are unlikely to contract measles. One dose is 93% effective at preventing measles.
It only takes a few days for antibodies to develop in response to the MMR vaccine. Within two to three weeks of vaccination, the immune system is ready to protect against measles.
Yes. It is safe for most people. However, a vaccine, like other medicines, can cause side effects in some people. The MMR vaccine can cause fever, mild rash, temporary pain or stiffness of the joints. More severe problems, such as seizures, bleeding problems or allergic reactions are very rare. Getting MMR vaccine is much safer than getting measles, and most people do not have any problems with the vaccine.
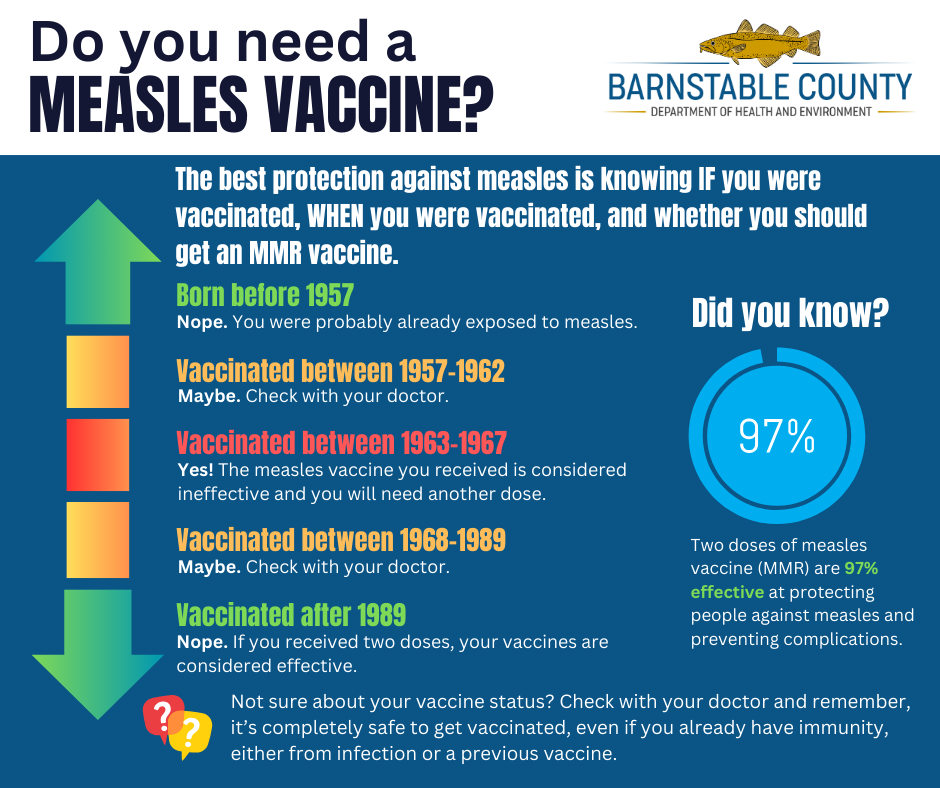
This depends on a variety of factors including age, health, vaccination status, and risk level. It is a decision that should be made with the guidance of trusted healthcare professionals. Anyone who questions their vaccination status should talk to their doctor about whether to pursue an MMR vaccine.
General guidance includes the following:
If you cannot find your vaccine records, you should get vaccinated. The MMR vaccine is safe to receive even if you already have immunity to measles, mumps, or rubella.
No. Persons with evidence of presumptive immunity do not need any further vaccines. No “booster” doses of MMR vaccine are recommended for either adults or children. There are no recommendations for a 3rd dose of MMR vaccine to improve protection against measles. People are considered to have life-long immunity once they have received the recommended number of MMR vaccine doses or have other evidence of immunity.
Because measles is more common in other parts of the world, people who travel to other countries should make sure that they are protected before traveling.
Talk to your doctor if you have questions about measles, mumps, and rubella (MMR) vaccine. Many pediatricians, doctor’s offices, and pharmacies offer measles vaccines. In addition to those locations, you can call and schedule an MMR vaccine with:
READ THE MA DPH CLINICAL ADVISORY. AVAILABLE HERE
Acceptable evidence of presumptive immunity against measles includes at least one of the following:
Although birth before 1957 is considered acceptable evidence of measles immunity, healthcare facilities should consider vaccinating unvaccinated personnel born before 1957 who do not have other evidence of immunity with 2 doses of MMR vaccine (minimum interval 28 days).
Prior to hiring, healthcare facilities should require 2 doses of MMR vaccine at the appropriate interval for unvaccinated healthcare personnel regardless of birth year if they lack laboratory evidence of measles immunity.
Persons without evidence of presumptive immunity and no contraindications to MMR vaccine can be vaccinated without testing. Persons without evidence of presumptive immunity might be considered for testing for measles-specific IgG antibody, but testing is not needed prior to vaccination, and insurance coverage for it varies.
ACIP does not recommend measles antibody testing after MMR vaccination to verify the patient’s immune response to vaccination.
Two documented doses of MMR vaccine given on or after the first birthday and separated by at least 28 days is considered evidence of presumptive immunity, according to ACIP. Documentation of appropriate vaccination supersedes the results of serologic testing for measles, mumps, rubella, and varicella.
First, make sure all your patients are fully vaccinated according to the U.S. immunization schedule.
In certain circumstances, MMR vaccine is recommended for infants aged 6 through 11 months. Give infants this age a dose of MMR vaccine before international travel, or travel to areas of the US with a current outbreak. Do not count any dose of MMR vaccine as part of the 2-dose series if it is administered more than 4 days before a child’s first birthday. Instead, repeat the dose when the child is 12 months.
If a young child is travelling internationally or to an area in the US with an outbreak, you might consider vaccinating children age 12 months and older at the minimum age (12 months, instead of 12 through 15 months) and giving the second dose 4 weeks later (at the minimum interval) instead of waiting until age 4 through 6 years.
Finally, remember that infants too young for routine vaccination and people with medical conditions that prevent them from being immunized for measles, depend on high MMR vaccination coverage among those around them for protection. Be sure to encourage all your patients and their family members to get vaccinated if they are not immune.
MMR can be given to children as young as 6 months of age who are at high risk of exposure such as during international travel or a community outbreak. However, doses given BEFORE 12 months of age cannot be counted toward the 2-dose series for MMR vaccination.
Yes. Healthcare personnel (HCP) with 2 documented doses of MMR vaccine are considered to be immune regardless of the results of a subsequent serologic test for measles, mumps, or rubella. Documented age-appropriate vaccination supersedes the results of subsequent serologic testing. In contrast, HCP who do not have documentation of MMR vaccination and whose serologic test is interpreted as “indeterminate” or “equivocal” should be considered not immune and should receive 2 doses of MMR vaccine (minimum interval 28 days). ACIP does not recommend serologic testing after vaccination. For more information, see ACIP’s recommendations on the use of MMR vaccine at www.cdc.gov/mmwr/pdf/rr/rr6204.pdf, page 22.
People with medical conditions that contraindicate measles immunization depend on high MMR vaccination coverage among those around them to protect them. To help prevent the spread of measles virus, make sure all your staff and patients who can be vaccinated are fully vaccinated according to the U.S. immunization schedule. Also, encourage patients to remind their family members and other close contacts to get vaccinated if they are not immune.
If patients who cannot get MMR vaccine are exposed to measles, CDC has guidelines for immune globulin for post-exposure prophylaxis which can be found at www.cdc.gov/mmwr/pdf/rr/rr6204.pdf
MMR vaccine given to susceptible individuals within 72 hours of initial measles exposure can reduce the risk of getting sick or reduce the severity of symptoms.
Another option for exposed, measles-susceptible individuals at high risk of complications who cannot be vaccinated is to give immunoglobulin (IG) within 6 days of exposure. Do not administer MMR vaccine and IG simultaneously, as the IG invalidates the vaccine.
More information on post-exposure prophylaxis for measles can be found in the 2013 ACIP guidance at www.cdc.gov/mmwr/pdf/rr/rr6204.pdf, page 24.

The US 2025 Measles Dashboard is an interactive tool offering real-time insights into the current measles outbreak across the United States.
This dashboard provides up-to-date data on reported cases, county-level immunization coverage where available, and outbreak information, enabling public health officials, healthcare providers, and the general public to monitor and respond effectively to the evolving situation.
Massachusetts Department of Public Health website
Measles Outbreak Fact Sheet-June 2019 (cdc.gov)
Measles Cases and Outbreaks | CDC
The Massachusetts Department of Public Health, Bureau of Infectious Disease and Laboratory Sciences at (617) 983-6800 or on the MDPH Website.
Boston providers and residents may also call the Boston Public Health Commission at (617) 534-5611.
CDC National Contact Center Hotline (Monday–Friday, 8 AM – 8 PM):
The best protection against measles is knowing IF you were vaccinated, WHEN you were vaccinated, and whether you should get a Measles, Mumps, & Rubella (MMR) vaccine. Most people who […]
Read MoreMeasles, a highly contagious viral disease, has significantly impacted communities worldwide throughout history. Understanding its past sheds light on the importance of vaccination and continued public health efforts. Early Measles […]
Read More