Pertussis (Whooping Cough)
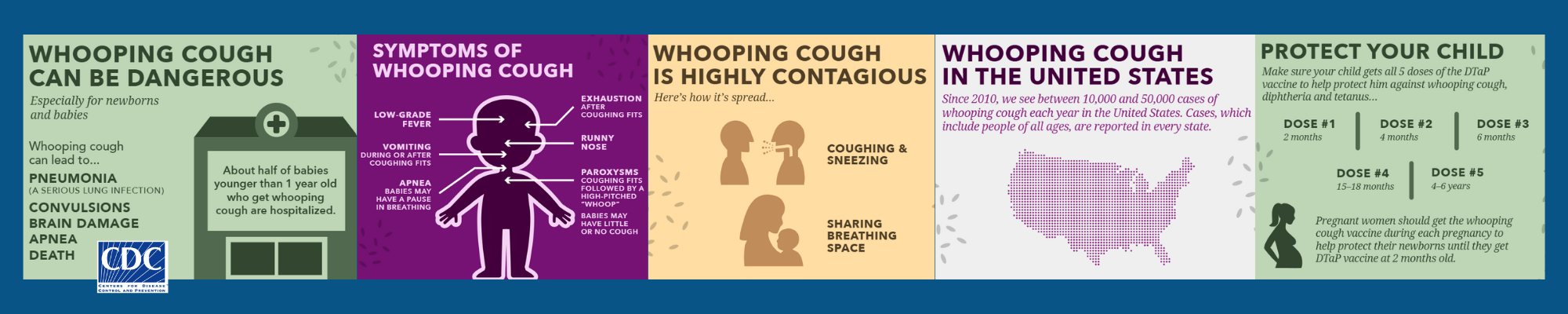
Pertussis, also called “whooping cough”, is a common and highly contagious bacterial respiratory infection that can be dangerous, especially to young infants. In older children, teens, and adults, the symptoms of pertussis are often mild, but can last for weeks or months.
Pertussis lives in the nose, mouth, and throat of an infected person and is spread through the air by sneezing, coughing, or talking. Pertussis can also live on surfaces, so touching a tissue or sharing a cup used by someone with pertussis can effectively spread the disease. Pertussis can exacerbate the symptoms of people with pre-existing moderate-to-severe asthma, immunocompromising conditions, and possibly other conditions.
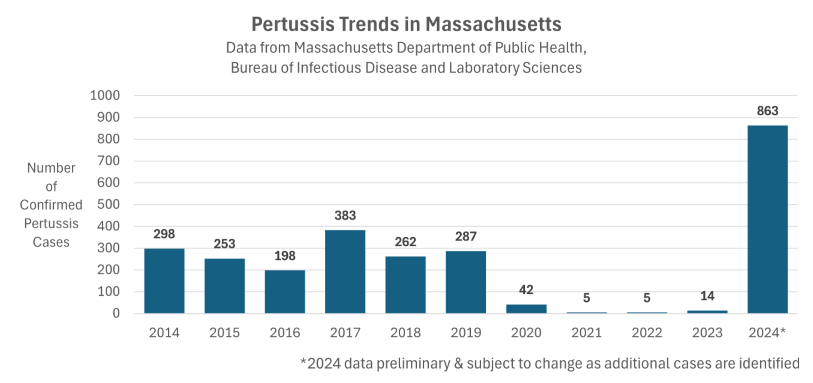
During the COVID-19 pandemic, respiratory protections like masking and remote work/learning led to decreases in transmission of pertussis. Post-pandemic, pertussis is back on the rise in Massachusetts and nationally. Pertussis was first identified on the Cape & Islands in Barnstable County in June 2024. In Dukes County, pertussis was first identified in November. To-date, there have been no cases in Nantucket County.
Read the MA DPH Clinical Advisory regarding pertussis in Massachusetts >>>
Related: Pertussis (Whooping Cough) Cases Rising in Barnstable County| 12/17 Advisory >>>
This page includes information about:
- Symptoms of pertussis
- Prevention
- Pertussis epidemiology specific to the Cape & Islands
- 2024 week-to-week case counts
- Trends by age
- Trends by year and county
- Information for Healthcare Providers
- Optimal timing for pertussis diagnostic testing
- Requested actions
- Help stop the spread
- Information for School Health Personnel
- Policy and procedure recommendations before a case is identified
- What to do when you have pertussis in your school
- Recommendations for after cases or outbreaks occur
- Pertussis Cough Illness Screening Tool for Schools
Symptoms, Diagnosis, and Treatment of Pertussis
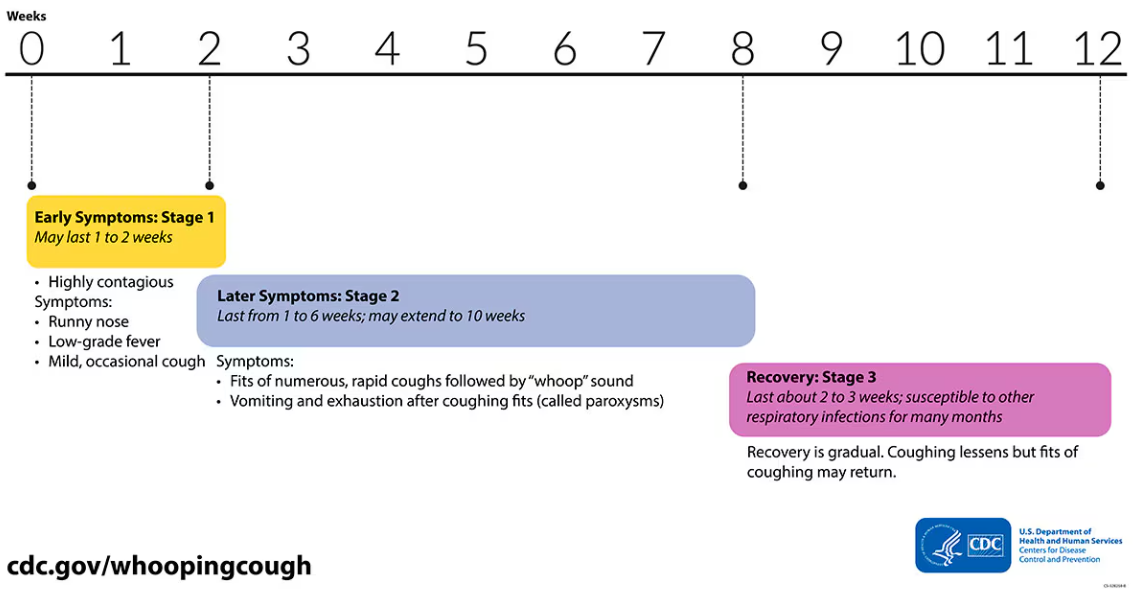
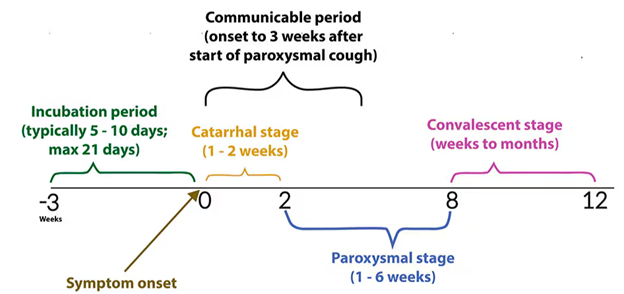
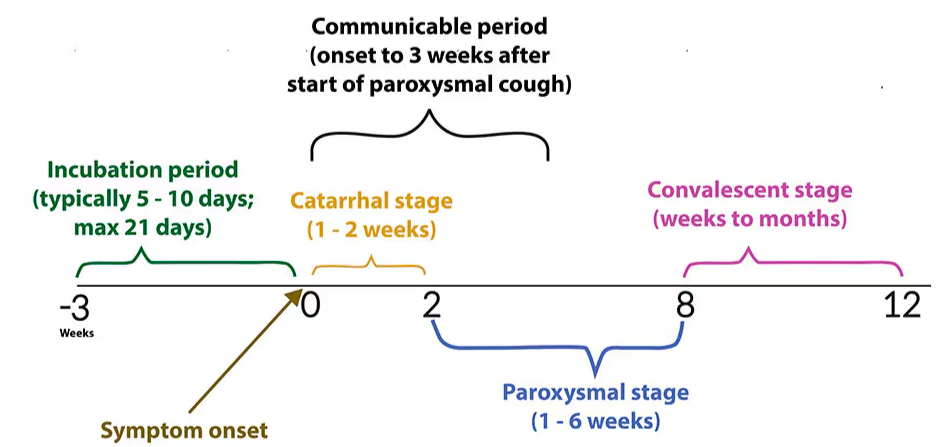
Pertussis has three stages, resulting in a progression of symptoms that can last weeks to months if left untreated:
- Week 1-2 (Catarrhal stage): Symptoms mimic the common cold including runny nose, sneezing, and mild cough.
- Weeks 2-8 (Paroxysmal stage): Symptoms progress to a worsening, miserable cough that can cause such severe coughing fits that people may become blue in the face or make a “whoop” sound as they try to catch their breath. Patients can become exhausted or begin vomiting from such severe coughing. Coughing attacks occur frequently at night.
- Weeks 8-12 (Convalescent stage): Symptoms gradually improve with less persistent coughing fits that disappear in 2 to 3 weeks.
Early Diagnosis and Treatment are Essential
Without antibiotic treatment, people who are sick with pertussis are most infectious to others in the first 3 weeks of symptoms. So early diagnosis and treatment are essential. After 5 days of antibiotic treatment, the sick person is no longer contagious to anyone else. Early administration of antibiotics can also reduce the length and severity of symptoms.
If You Have Been Exposed to Pertussis, Talk to Your Doctor about Treatment Before Symptoms Start
If someone has close contact with someone with pertussis and they get infected, symptoms usually start showing up 5 to 10 days later but could take as long as 21 days. In that window, there is the option to take 5 days of antibiotics to altogether prevent getting pertussis at all. This is recommended for household contacts who are highly likely to get pertussis from their family member. This can also be very important if you are high risk for severe illness or could have contact with high risk individuals (see below about infants and pregnant women). If you have been exposed to pertussis, call your doctor and ask about “prophylaxis“.
Pertussis is Especially Concerning for Infants
In babies, pertussis can cause breathing problems, pneumonia, and swelling of the brain (encephalitis), which can lead to seizures and brain damage. In rare cases pertussis can even be fatal, especially in very young infants.
The following video from the Mayo Clinic, while difficult to watch, shows the effects of pertussis in a young infant: Infant girl with whooping cough (youtube.com)
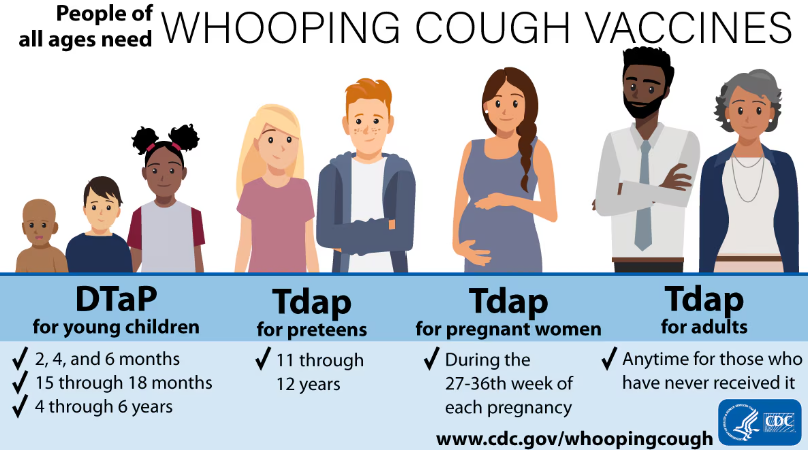
Pregnant Women in their Third Trimester
It is important to protect and/or treat pregnant women so that they do not inadvertently infect their infants post-birth.
If you think you or a loved one has pertussis, or has been exposed to pertussis, talk to a doctor as soon as possible!
Pertussis can be PREVENTED!
Pertussis vaccines are the best way to protect against whooping cough! The Centers for Disease Control and Prevention recommends pertussis (whooping cough) vaccination for everyone.
Talk to a vaccine provider if you have questions about pertussis vaccine. Many pediatricians, doctor’s offices, and pharmacies offer pertussis vaccines. Barnstable County Public Health Nurses also offer the vaccine. Appointments are available on Tuesdays and Thursdays 8:30am to 4:00pm. To schedule an appointment, call (508) 375-6617.
In the following video, Michael Forbes, MD, an intensivist in the pediatric intensive care unit at Akron Children’s Hospital, discusses the symptoms of this disease, as well as its treatment and prevention.
How to Identify a Close Contact for Pertussis
Pertussis Epidemiology on the Cape & Islands
Pertussis Trends by Year and County
YTD = Year-to-Date. Last updated March 10, 2025
Year assigned is based on the date symptoms started. If a patient is unable to be interviewed to determine symptom onset date, the date the individual first tested positive is used. Case counts in 2024 are considered preliminary and subject to change as additional cases are identified. Data is expected to be in its final form in March. Includes confirmed cases. Learn more about how public health officials classify cases here: Pertussis National Case Classification.
Because Dukes County and Nantucket County have smaller year-round populations (<25,000 people), years with fewer than 5 cases are reported as “<5” to preserve patient confidentiality. Only Barnstable County data is presented in this epidemiologic curve because fewer than 5 cases of pertussis occurred in Dukes County in 2024.
| Year (Newest to oldest) | Barnstable County (Cape Cod) | Dukes County (Martha's Vineyard & Elizabeth Islands) | Nantucket County (Nantucket, Tuckernuck) |
|---|---|---|---|
| 2025 (Year to-date) | 10 | - | - |
| 2024 (Preliminary; subject to change as additional cases are reported) | 33 | <5 | 0 |
| 2023 | 1 | 0 | 0 |
| 2022 | 0 | 0 | 0 |
| 2021 | 1 | 0 | 0 |
| 2020 | 0 | 0 | 0 |
| 2019 | 7 | 0 | 0 |
| 2018 | 3 | <5 | <5 |
| 2017 | 7 | 0 | 0 |
| 2016 | 0 | 0 | 0 |
| 2015 | 10 | <5 | 0 |
| 2014 | 42 | 0 | 0 |
| 2013 | 1 | <5 | 0 |
| 2012 | 23 | <5 | <5 |
| 2011 | 3 | 0 | 0 |
| 2010 | 5 | 0 | 0 |
Historical Pertussis Trends
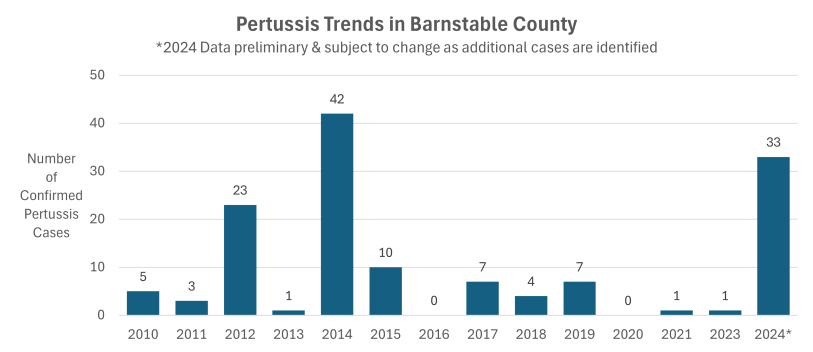
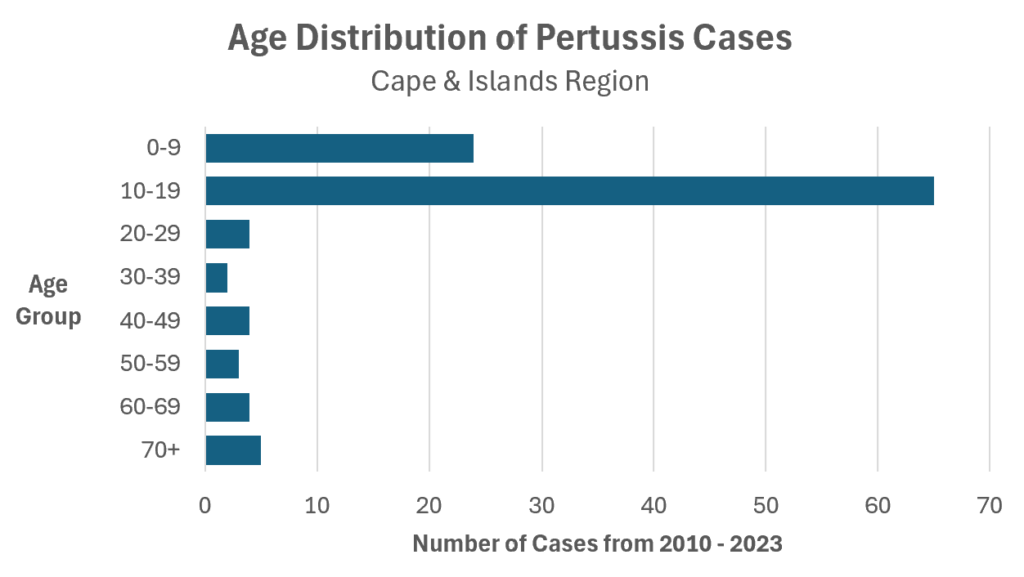
By Age: Since 2010, approximately 80% of diagnosed and reported pertussis cases on the Cape & Islands have been in kids and teenagers.
Information for Health Care Providers
Pertussis, also known as “whooping cough,” is a highly contagious, vaccine preventable respiratory illness caused by the bacteria Bordetella pertussis. Following a significant decline during the COVID-19 pandemic, in 2024 cases of pertussis in Massachusetts exceeded pre-pandemic levels, particularly among adolescents. The Massachusetts Department of Public Health has published two Clinical Advisories:
- Pertussis Cases Increasing in Massachusetts, August 20, 2024
- Increase in Mycoplasma Pneumonia and Pertussis Cases in Massachusetts, November 8, 2024
Actions Requested:
1) SUSPECT: Maintain a high index of suspicion for pertussis to identify those infected. Massachusetts has seen more pertussis in 2024 than the previous 6 years combined. It is recommended that providers consider pertussis in any patient with consistent symptoms, regardless of vaccination status. See more about differences in clinical presentations here: CDC Clinical Signs of Pertussis.
- Symptoms of pertussis include:
- Week 1-2 (Catarrhal stage): Symptoms mimic other upper respiratory infections including coryza, sneezing, low-grade fever, and/or a mild occasional cough. Infants may present as apnea, gagging, gasping, or bradycardia without cough. Infected persons are highly contagious in this stage of illness.
- Weeks 2-8 (Paroxysmal stage): Classic presentation is characterized by paroxysms of numerous, rapid coughs, long inspiratory effort with a high-pitched “whoop” at the end of paroxysmal cough, cyanosis, exhaustion, and/or post-tussive vomiting. Paroxysmal attacks occur frequently at night, with an average of 15 attacks per 24 hours. They increase in frequency during the first 1 to 2 weeks. The attacks remain at the same frequency for 2 to 3 weeks, then gradually decrease. Vaccinated individuals, adults and adolescents may have atypical presentation of prolonged cough without paroxysms or “whoop”.
- Weeks 8-12 (Convalescent stage): Symptoms gradually improve with less persistent coughing fits that disappear in 2 to 3 weeks.
- Atypical presentations: Symptoms in adults and adolescents, as well as vaccinated individuals, may be less severe and may not include the characteristic paroxysmal cough or “whoop”. Symptoms may be defined as a prolonged cough.
- Patients at high risk for severe sequelae include infants <1 year of age (particularly those <6 months of age), immunocompromised individuals, individuals with chronic lung disease (including asthma and cystic fibrosis), individuals with neuromuscular disorders that prevent or reduce the ability to clear secretions, or unimmunized or under-immunized children.
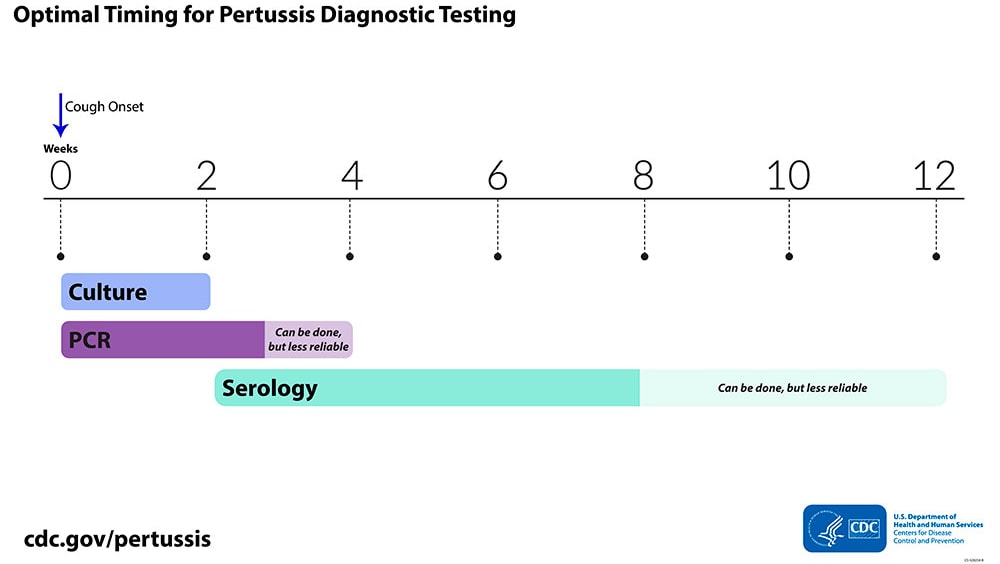
2) TEST patients who have symptoms of pertussis. See the MA DPH Pertussis Clinical Advisory for specific testing recommendations in Massachusetts. Contact the State Public Health Lab at 617-983-6607, M-F 8am-4pm, with any questions regarding Bordetella pertussis testing.
- PCR with an NP swab may be the more clinically useful option in early illness as it is readily available from hospital and commercial labs and results are available quickly.
- Culture with an NP swab requires specific media and special ordering from the State Public Health Lab.
- Serology for confirmatory testing of pertussis infection is available through the State Public Health Lab and is only validated for individuals 11 years old and older.
3) TREAT promptly. Specific treatment recommendations are outlined in CDC Treatment Guidelines. Antibiotic treatment is recommended for people with a diagnosis of pertussis and cough duration of <3 weeks. Macrolides (e.g., azithromycin) are generally first line treatment for pertussis. The earlier antibiotics are started, the more effective they are in preventing disease transmission to others. The symptoms of pertussis may be ameliorated if treatment is begun early, during the catarrhal stage. If begun later in the course of illness, treatment will decrease the infectious period but may not decrease the duration of cough or severity of disease. Consider treating prior to test results if the patient has consistent symptoms AND:
- The patient has a known exposure to pertussis, OR
- The patient has consistent symptoms and is at high risk for severe or complicated disease, OR
- The patient has or will have contact with someone at high risk for severe disease
4) ISOLATE: Inform patients with pertussis that they need to isolate and NOT participate in public activities (including work/school/camp) until they have completed 5 days of appropriate antibiotic treatment. They can return to activities on the 6th day after starting treatment.
5) PROPHYLAX household contacts: Household contacts have significant face-to-face exposure and are the most likely to become infected with pertussis, regardless of vaccination history, and are easily identified by providers for post-exposure prophylaxis antibiotics. To be effective, post-exposure prophylaxis must be given within 21 days of exposure. For infants <1 year, particularly those <6 months, consider prophylaxis within 42 days of exposure. Contact MA DPH for consultation at 617-983-6800.
6) EDUCATE about contact tracing: Tell your patient that if they are positive for pertussis, public health authorities will be contacting them to assess where they were exposed and contacts that could benefit from prophylaxis.
7) PROPHYLAX close contacts identified by public health: If public health refers a patient to their doctor for prophylaxis, please treat them unless contraindicated for that patient. Public health officials are trained to apply state guidelines for assessing close contacts. Contacts may not be informed of the exact time and place they were exposed to protect the original patient’s confidentiality. If a patient has been notified as being a close contact, public health recommends antibiotic prophylaxis to prevent spread.
- Close contacts with symptoms should be treated with antibiotics as soon as possible and isolated until they have completed 5 days of antibiotic treatment. Ideally these patients are also tested for pertussis so that public health can initiate the next level of contact tracing efforts. Regardless of testing, patients should be treated as pertussis cases when they have a known exposure and consistent symptoms.
- Close contacts without symptoms ideally should receive prophylactic antibiotics within 21 days of exposure to prevent infection. So long as they are asymptomatic, close contacts do not need to be isolated. If close contacts refuse antibiotic prophylaxis, they should be educated on symptom monitoring and to seek care immediately if early pertussis symptoms develop (runny nose, sneezing, low-grade fever, cough). If there is a shortage of antibiotics, prioritize contacts that are high-risk for severe illness or who will be in contact with high-risk individuals (e.g. a daycare provider, a healthcare provider, etc
8) REPORT information to public health authorities as soon as possible especially if the infected patient has been in settings like daycares, healthcare facilities, long-term care, jails, schools, or camps where public health investigation and intervention can prevent the spread of disease. Report to your Local Board of Health or the Massachusetts Department of Public Health at (617) 983-6800.
- Respond to public health authorities requesting information expeditiously. Public health authority lies with where a patient resides so expect to be contacted by the Local Board of Health where the patient lives. Local Boards of Health are expressly permitted to receive medical record information for the purposes of disease control (see MA DPH HIPAA Memo.) Timely investigation is critical to disease control.
- Report clusters and outbreaks. Healthcare providers are required to report illness believed to be part of a suspected or confirmed cluster or outbreak within 24 hours (105 CMR 300.134).
- Inform Infection Control, if available, of any patients seen in your clinic diagnosed with pertussis.
Information for School Health Personnel
We recommend schools have policies and procedures in place for:
- Tracking and managing staff, student, and volunteer vaccination records.
- Excluding staff and students that are diagnosed with pertussis.
- Implementing a parent notification system following an exposure. Call MA DPH Epidemiology (617-983-6800) for a template letter.
- Tracking the number of student and staff absences due to similar symptoms or cause.
What to do when you have pertussis in your school:
- REPORT lab-positive cases to your Local Board of Health or MA DPH Epidemiology (617-983-6800).
- EXCLUDE lab-positive case(s) from school until they have finished a 5-day course of antibiotic therapy. If a case has been diagnosed by a provider but the lab is pending, most cautious approach would be to ask they remain out of school until lab returns. If case declines antibiotic therapy, your Local Board of Health will provide dates of exclusion based on symptom onset (usually 21 days after cough onset).
- IDENTIFY CLOSE CONTACTS: Work with your Local Board of Health or MA DPH Epidemiology (617-983-6800) to determine the infectious period and identify close contacts, especially contacts at high risk for severe disease. You may need to interview teachers, coaches, and/or staff to determine who was a close contact. A tool to identify who is a close contact to a pertussis case can be found on page 19 of the Pertussis Guide to Surveillance, Reporting and Control.
- ASSESS the symptoms of close contacts. Notify teachers or coaches who have had a case in their class or in their sports team to refer other coughing children to the nurse’s office for evaluation.
- EXCLUDE symptomatic close contacts. Close contacts that develop symptoms consistent with pertussis should be treated as cases. Refer them for medical evaluation, testing, and treatment, and exclude until they have finished a 5-day course of antibiotic therapy or, if case declines, after 21 days from their onset of cough. Report any excluded symptomatic contacts to your Local Board of Health.
- NOTIFY: Distribute a notification letter and FAQ sheet to potentially exposed persons at a minimum. Wider notification of unexposed persons may be advisable depending on the situation.
- Template notification letters: call MA DPH (617-983-6800).
- FAQs: available in multiple languages are at bottom of webpage here.
- In situations of pertussis outbreaks, consider resending notification letters every 45 days to exposed groups or posting pertussis information on your school website.
- RECOMMEND PROPHYLAXIS for asymptomatic close contacts: In the school setting, antibiotic prophylaxis should be limited to those defined as close contacts while continuing to monitor for additional cases of cough illness. In general, antibiotic prophylaxis is not usually indicated for an entire classroom where there is only one lab-positive case. However, there may be some rare exceptions to this, such as special needs classrooms where there is a great deal of close contact, or many high-risk students, or small classrooms of very young children.
- MONITOR asymptomatic close contacts. It is not usually indicated to exclude asymptomatic unvaccinated or under-vaccinated contacts. Continue monitoring symptoms in exposed individuals for 21 days from last exposure.
- IN AN OUTBREAK, EXPAND SCREENING: School nurses seeing an increased number of students with a cough illness during a pertussis outbreak should be vigilant for students, staff, and volunteers with new symptoms.
- PREVENT: Reinforce cough etiquette education and hand hygiene education to reduce the spread of illness in the school. Refer under or unimmunized children for vaccination. Appointments can be made for pertussis vaccination with the Barnstable County Public Health Nurse (Tues/Thurs appointments) by calling 508-375-6617.
After cases or outbreaks occur:
- Evaluate your school’s response.
- Develop action plans to address identified areas of concern regarding school’s readiness and response.
- Don’t hesitate to use Barnstable County Department of Health and Environment as a resource to review outbreak response or support training needs. Contact us at (774) 330-3001.
Pertussis Cough Illness Screening Tool
Barnstable County Department of Health and Environment has developed a cough illness screening tool for school nurses to use when evaluating children who visit their office during the school day. The tool makes parents aware that the child is exhibiting persistent cough with symptoms that are consistent with pertussis. After the child is seen by the school nurse and the screening is conducted, the following letter can be sent home to provide detailed information that can be passed along to the child’s healthcare provider.
Download the letter (PDF Format) HERE >>>
For an editable version of the screening tool, please contact lea.hamner-contractor@capecod.gov.